What is the Prostate Health Index?
Share
Each year, over 250,000 men in the U.S. are told they have prostate cancer. Many others face unnecessary biopsies because high prostate specific antigen (PSA) levels don’t always mean cancer. This causes stress, discomfort, and added medical costs.
To improve accuracy and reduce unnecessary procedures, doctors now use the Prostate Health Index (PHI), a more advanced blood test that combines three PSA markers.
PHI provides a clearer assessment of prostate cancer risk, helping men and their doctors make more confident decisions about next steps.
To know more about how PHI works, what it measures, and why it matters, keep reading.
What Is the Prostate Health Index (PHI)?
The Prostate Health Index (PHI) is an FDA-approved blood test that combines three PSA measurements to provide a more accurate prostate cancer risk assessment.
Rather than relying on a single PSA value, it calculates a composite score using total PSA, free PSA, and [-2]proPSA levels. This three-pronged approach offers significantly better specificity than traditional PSA testing alone.
PHI received FDA approval in 2012 and has since gained endorsement from multiple cancer organizations including the National Comprehensive Cancer Network. The test specifically helps distinguish between benign prostate conditions and potentially cancerous ones.
This improved accuracy reduces unnecessary biopsies while maintaining high cancer detection rates.
How PHI Is Calculated
The PHI formula combines three biomarkers in a specific mathematical relationship:
PHI = ([-2]proPSA / free PSA) × √(total PSA)
This calculation leverages the fact that cancer cells produce different PSA patterns compared to healthy prostate tissue.
The formula works because higher total PSA and [-2]proPSA levels combined with lower free PSA typically indicate increased cancer risk.
Meanwhile, the square root of total PSA in the formula helps normalize the score across different PSA ranges.
This mathematical approach creates a more nuanced risk assessment than any single PSA measurement could provide.
Why PHI Was Developed
Traditional PSA testing suffers from poor specificity, which leads to many false positives. Studies show that only about 25% of men with elevated PSA actually have prostate cancer. This poor accuracy creates significant overdiagnosis and unnecessary anxiety for patients.
Recognizing these limitations, researchers developed PHI to improve diagnostic precision. Multiple clinical studies have validated PHI's superior performance over standard PSA testing.
According to a study, PHI achieved better specificity with an area under the curve of 0.70 compared to 0.65 for free PSA and 0.53 for total PSA alone.
Building on this research, another study further confirmed that PHI predicts clinically significant cancer more accurately than traditional PSA measurements.
These studies established PHI's role in reducing unnecessary biopsies while maintaining cancer detection sensitivity. The result is more targeted healthcare that focuses resources on patients who truly need intervention.
Clinical Use & Target Population of PHI
PHI works best for specific patient populations where traditional PSA creates diagnostic uncertainty. The ideal candidates are men aged 50 and older with total PSA levels between 4-10 ng/mL and non-suspicious digital rectal exams. This "gray zone" represents where most diagnostic confusion occurs.
Within this target population, the test integrates into established clinical guidelines as a decision-support tool.
The National Comprehensive Cancer Network now includes PHI in their prostate cancer screening recommendations. Many urologists have adopted PHI to guide biopsy decisions rather than relying solely on PSA levels.
Beyond initial screening, PHI also helps monitor men on active surveillance who have low-risk prostate cancer. Changes in PHI scores over time can indicate whether cancer is becoming more aggressive.
This monitoring capability adds another layer of safety for men choosing observation over immediate treatment.
How to Interpret PHI Scores
PHI scores correlate with specific cancer risk percentages that help guide clinical decisions. Understanding these ranges helps both patients and doctors make informed choices about next steps.
The scoring system provides four clear risk categories:
- Below 27: Approximately 10% cancer risk
- 27-36: Approximately 16% cancer risk
- 36-55: Approximately 33% cancer risk
- 55 and above: Approximately 50% cancer risk
Lower PHI scores suggest that elevated PSA is likely due to benign conditions like enlargement or inflammation.
Conversely, higher scores indicate increased probability that cancer is present. These percentages help patients understand their individual risk level rather than dealing with diagnostic uncertainty.
Benefits & Limitations of Prostate Health Index
The Prostate Health Index offers valuable insight for prostate cancer screening, but like any tool, it has Key Benefits and important limitations that should be understood.
Key Benefits
PHI helps lower the number of unnecessary biopsies. Studies show it can reduce procedures by 30–36%. This means less worry, pain, and risk from invasive tests. Men with low PHI scores can feel safer choosing to monitor rather than have an immediate biopsy.
Additionally, the test provides better risk stratification than traditional PSA alone. This improved accuracy helps identify men who truly need aggressive evaluation versus those who can safely delay or avoid biopsy.
PHI also supports active surveillance monitoring by tracking changes in cancer aggressiveness over time.
Important Limitations
Despite its improvements, PHI isn't 100% accurate and can produce false negatives or positives. Some men with low scores may still have cancer, while others with high scores may not.
The test should always be interpreted alongside other clinical factors and patient history.
Cost and insurance coverage remain additional barriers for some patients. Not all insurance plans cover PHI testing, making it expensive for out-of-pocket payment. Access may also be limited in certain geographic areas or healthcare systems.
Furthermore, pre-analytical factors can affect results accuracy. Recent digital rectal exams, biopsies, or ejaculation can temporarily alter PSA levels. Patients need proper preparation and timing to ensure reliable results.
PHI vs Other Advanced Tests
This section provides a simple comparison of PHI and other advanced tests to help guide decision-making.
|
Test |
Biomarkers |
Advantages |
Limitations |
|
PHI |
3 PSA variants |
FDA-approved, well-studied |
Limited to PSA pathway |
|
4Kscore |
4 proteins + clinical data |
Includes additional factors |
More complex, newer |
|
PCA3 |
Urine-based |
Non-invasive collection |
Requires urologist visit |
|
IsoPSA |
PSA structural analysis |
Novel approach |
Limited clinical data |
|
EpiSwitch PSE |
Epigenetic markers |
Different biological pathway |
Research stage |
PHI offers the advantage of using established PSA measurements in a refined calculation. Other tests may include broader biomarker panels but often lack PHI's extensive clinical validation.
The choice between tests often depends on individual patient factors and physician preference.
Frequently Asked Questions
When should I consider PHI testing?
PHI is most beneficial when your total PSA falls between 4-10 ng/mL and your doctor is considering a biopsy. It's particularly useful if you want to avoid unnecessary procedures or need help making biopsy decisions.
Is PHI covered by insurance?
Coverage varies significantly by insurance provider and plan. Medicare covers PHI in certain circumstances, but private insurance coverage differs widely. Check with your insurance company and healthcare provider about coverage before testing.
Is the prostate health index a blood test?
Yes, PHI requires only a simple blood draw, similar to standard PSA testing. The same blood sample can measure all three PSA components needed for the calculation.
How do I prepare for the test?
Avoid ejaculation for 48 hours before testing. Don't schedule PHI immediately after digital rectal exams or prostate procedures. Follow your doctor's specific instructions about timing and preparation.
What should I discuss with my doctor about the results?
Review your individual risk percentage and what it means for your specific situation. Discuss whether biopsy is recommended, active surveillance options, and follow-up testing schedules. Consider your personal preferences about treatment versus monitoring approaches.
Take Control of Your Prostate Health Today
Understanding your prostate cancer risk is just the first step in comprehensive prostate health management. While PHI testing provides valuable diagnostic insight, maintaining optimal prostate health requires consistent attention and proactive care.
Artagia Med’s Sonic Prostate Massager offers a non-invasive way to support prostate wellness through targeted therapeutic massage. This FDA-cleared device helps promote healthy circulation and complements your overall health plan.
For extra support, take The Ultimate Prostate Health Supplement. It’s made with ingredients that help reduce inflammation, support hormone balance, and improve urinary flow.
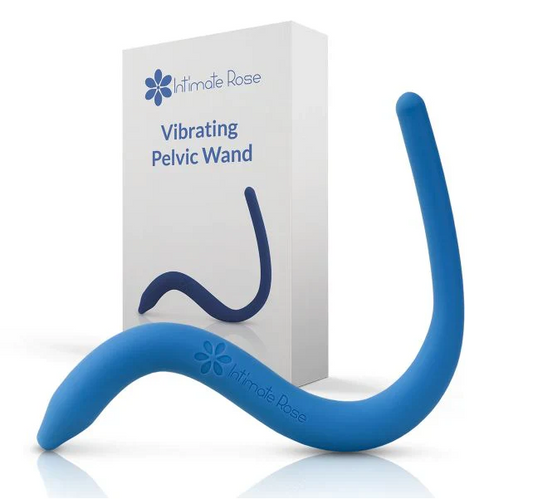
You can also use a pelvic floor wand to strengthen the muscles that support your prostate and bladder, which is important for long-term health.
Take charge of your prostate health today. Order your complete wellness tools now and start building a stronger, healthier future.