Chronic Prostatitis/CPPS: A Comprehensive Guide to Understanding and Finding Relief
Share
Chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) affects between 2% and 16% of men worldwide. This makes it one of the most common urological conditions in younger men yet it remains widely misunderstood and underdiagnosed.
For many, finding answers takes years, with visits to different doctors and treatments that only partly help.
This guide aims to make CP/CPPS easier to understand. We’ll break down what it is, explore possible causes, and share practical, evidence-based treatments that have helped many men feel better.
You’ll also learn why managing this condition requires a different approach than most medical issues.
What is Chronic Prostatitis/CPPS?
Chronic prostatitis, also known as chronic pelvic pain syndrome (CP/CPPS), is exactly what it sounds like, ongoing pelvic pain that lasts for at least three months. It’s often linked with urinary or ejaculatory symptoms but happens without any bacterial infection.
Unlike bacterial prostatitis, which responds to antibiotics, CP/CPPS doesn't improve with typical infection treatments.
Doctors call it a "diagnosis of exclusion," meaning they have to rule out other conditions, like bacterial prostatitis, urinary tract infections, or prostate cancer, before confirming CP/CPPS.
This process can take time and may involve several tests, urine samples, and sometimes even a prostate biopsy.
To better understand and manage the condition, doctors often use the NIH classification system, which places CP/CPPS in Category III. They may also use the UPOINT system, which breaks symptoms into different categories to help create a more personalized and targeted treatment plan.
Causes of Chronic Prostatitis/CPPS
Many factors can contribute to CP/CPPS, and in most cases, multiple causes overlap to trigger or worsen symptoms.
Pelvic Floor Dysfunction
One of the leading explanations for CP/CPPS is pelvic floor muscle dysfunction. This happens when the muscles that support the bladder, prostate, and rectum stay chronically tense or uncoordinated.
Studies show that over half of men with CP/CPPS experience pelvic pain during or after ejaculation, and for many, this is the most troubling symptom.
This muscle tension can be caused by stress, physical strain, injury, or years of poor posture and movement habits.
Over time, the tight muscles may develop trigger points, which are small, hypersensitive knots that can radiate pain and irritate nearby nerves.
Neuropathic Inflammation
In some cases, the nerves become overly sensitive and keep sending pain signals even after the original cause has healed. This leads to a self-perpetuating cycle, where the nervous system “remembers” the pain, causing symptoms to continue, even when there’s no longer any actual tissue damage.
Psychological and Stress Factors
The mind-body connection also plays a key role in CP/CPPS. Emotional factors like anxiety, stress, and depression can show up physically as pelvic muscle tension.
Many men report that their symptoms worsen during times of stress and improve when they relax, further emphasizing how closely mental and physical health are linked
Chemical and Hormonal Theories
In addition to muscle and nerve-related causes, some researchers suggest that hormonal imbalances or chemical irritants in the urine might also contribute to symptoms.
Although these ideas are not as well-established as other theories, they may still play a supportive role in the development and persistence of CP/CPPS symptoms
Symptoms of Chronic Prostatitis/CPPS
CP/CPPS presents with a wide range of symptoms that can vary significantly between individuals:
- Perineal pain (between scrotum and rectum)
- Testicular aching or sharp pains
- Penis tip burning or discomfort
- Lower back pain
- Pain that waxes and wanes unpredictably
- Frequent urination, especially at night
- Sudden urgent need to urinate
- Difficulty starting urination
- Burning sensation during urination
- Painful ejaculation
- Erectile dysfunction
- Decreased libido and sexual satisfaction
- Chronic fatigue
- General muscle aches
- Anxiety and depression related to ongoing symptoms
Because symptoms can affect multiple systems, urinary, sexual, muscular, and emotional, CP/CPPS often impacts overall quality of life and can be challenging to manage without a comprehensive approach.
How to Treat Chronic Prostatitis/CPPS
Managing CP/CPPS requires a combination of physical, medical, and lifestyle strategies tailored to each individual’s symptoms and triggers.
Pelvic Floor Physical Therapy
This approach forms the cornerstone of modern CP/CPPS treatment. Specialized pelvic floor physical therapists use a combination of techniques to target the root causes of symptoms.
Myofascial release helps relax tight pelvic muscles, while biofeedback teaches proper muscle coordination.
In addition, targeted stretching exercises work to restore normal function, and breathing techniques are used to break the stress-tension cycle that often keeps symptoms going.
Targeted Medications
Medications can also help manage CP/CPPS symptoms. Alpha-blockers relax the muscles around the prostate and bladder, making it easier to urinate.
Muscle relaxants help ease tight pelvic floor muscles, while nerve pain medicines like gabapentin calm sensitive nerves that may be causing ongoing pain.
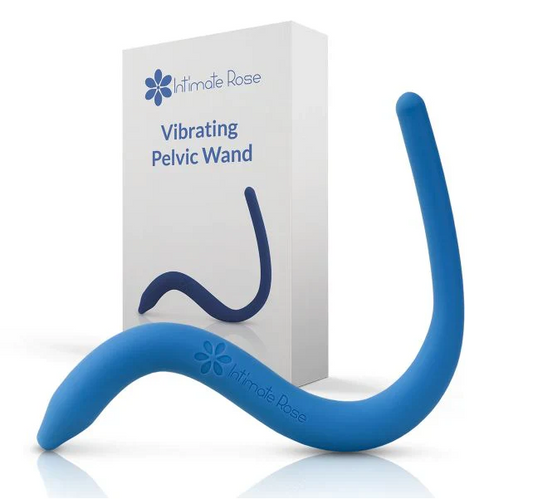
Prostate Massage and Therapeutic Devices
Prostate massage is based on the idea of "milking" the prostatic ducts to release trapped fluids and relieve congestion.
In addition to this, it may help relax trigger points in nearby pelvic floor muscles. Whether done professionally or with home devices, it can serve as a helpful addition to a broader, well-rounded treatment plan.
Lifestyle Modifications
Dietary changes often begin with avoiding common bladder irritants such as caffeine, alcohol, spicy foods, and artificial sweeteners. In parallel, heat therapy, through sitz baths or heating pads, can help relax tight pelvic muscles and enhance blood circulation.
To address the psychological factors that may worsen symptoms, stress management techniques like mindfulness, meditation, and regular exercise play an equally important role in the overall treatment approach.
Supplements and Alternative Therapies
Some men find relief with natural options like quercetin and bee pollen, which have shown promise in certain studies, though results remain mixed.
Acupuncture is another alternative that may help by calming nerve pathways and reducing stress.
As with any new treatment, it’s important to consult your healthcare provider before adding supplements or alternative therapies to your routine.
Why Is a Urologist So Important for Your Journey?
A urologist plays a central role in diagnosing and managing CP/CPPS. They have the expertise to rule out other conditions and perform tests like PSA levels, digital rectal exams, and post-void residual scans.
Once diagnosed, they can prescribe medications such as alpha-blockers, muscle relaxants, or nerve pain treatments based on your symptoms.
Just as important, experienced urologists understand that CP/CPPS often requires a team approach. They can refer you to pelvic floor therapists, pain specialists, or mental health professionals when needed.
With their guidance, you’ll have ongoing support, realistic expectations, and a clear path forward, even if it takes time to find the right treatment.
Frequently Asked Questions
Is CP/CPPS a permanent condition?
While CP/CPPS can be chronic, many men experience significant improvement or complete resolution with proper treatment. The key is finding the right combination of therapies and staying committed to the process.
Is there a link between CPPS and prostate cancer?
No established link exists between CP/CPPS and prostate cancer. This is a crucial myth to debunk, as the anxiety about cancer can actually worsen symptoms through increased stress and muscle tension.
What's the difference between CPPS and IC/BPS?
While both involve chronic pelvic pain, interstitial cystitis/bladder pain syndrome (IC/BPS) primarily affects the bladder, whereas CP/CPPS focuses on prostate and surrounding pelvic structures.
Find Your Path to Relief with Prostate Health Store
CP/CPPS doesn't have to define your life. With proper understanding, appropriate medical care, and the right tools, many men find significant relief from their symptoms.
For men committed to improving pelvic health, using specialized tools can enhance results and make pelvic floor exercises more effective and precise. The Sonic Prostate Massager from Prostate Health Store supports overall prostate wellness through therapeutic massage. This top-rated device promotes healthy blood flow and can complement your comprehensive treatment routine.
Additionally, our Prostate and Pelvic Floor Support Cushion provides daily comfort by reducing pressure during sitting, which is especially beneficial for men dealing with chronic pelvic pain.
For comprehensive nutritional support, the Ultra Prostate Health Formula with saw palmetto, pygeum, and stinging nettle root delivers 11 essential nutrients designed to support overall prostate function and wellness.
Order now and take control of your pelvic health with professional-grade tools made specifically for men’s wellness and comfort.