Can a Prostate Infection be Sexually Transmitted?
Share
When you’re feeling discomfort in your pelvic area, it’s normal to wonder if it might affect your partner, especially in a close relationship. One common question is whether a prostate infection can be sexually transmitted.
The short answer is that a prostate infection is not a sexually transmitted disease, but some types can be caused by sexually transmitted bacteria.
This guide will explain the different types of prostate infections, which ones may be linked to STIs, the symptoms to watch out for, and how to protect both yourself and your partner.
This information is for educational purposes only and should not replace medical advice from a healthcare professional.
What are the Different Types of Prostate Infections (Prostatitis)?
Not all prostate infections are created equal. Understanding the different types helps clarify the transmission question. Each type has distinct causes, symptoms, and implications for sexual health.
Acute Bacterial Prostatitis
Acute bacterial prostatitis is the most serious type of prostate infection and usually comes on suddenly, requiring urgent medical care.
It often starts when bacteria, commonly those that cause urinary tract infections, travel from the urethra or bladder into the prostate. In some cases, sexually transmitted bacteria may also be responsible.
Symptoms appear quickly and can be intense. Men may feel severe pelvic pain, have a high fever, chills, and trouble urinating. The pain can spread to the lower back and genitals, and many describe the illness as feeling like a bad case of the flu.
Chronic Bacterial Prostatitis
Chronic bacterial prostatitis condition is marked by repeated bacterial infections in the prostate, but unlike the acute form, symptoms appear slowly and last for a long time.
In some cases, it may be linked to bacterial STIs, with the same bacteria that cause acute infections also triggering this chronic form. However, the symptoms are usually milder and less intense than those of acute prostatitis.
Men often deal with recurring urinary tract infections, along with symptoms like frequent urination, a burning sensation while urinating, and pelvic discomfort that tends to come and go.
Chronic Pelvic Pain Syndrome (CPPS)
CPPS is the most common type of prostatitis. According to a study, 90% to 95% of prostatitis cases are CP/CPPS.
Unlike bacterial forms, CPPS isn’t caused by an infection. Instead, it involves chronic pain and inflammation without any bacteria present. Most importantly, it’s not sexually transmitted—so it cannot be passed to your partner through sexual contact.
The exact cause of CPPS is still unknown, but possible factors include pelvic muscle tension, nerve issues, autoimmune responses, or past infections that healed but left behind lingering inflammation.
Asymptomatic Inflammatory Prostatitis
This type is usually found during routine medical tests done for unrelated reasons. As the name suggests, it doesn’t cause noticeable symptoms that men can feel.
Because there are no symptoms and no bacterial infection, there’s no risk of sexual transmission. It’s essentially inflammation of the prostate without pain or an infectious cause.
STIs That Can Cause Prostatitis
When sexually transmitted infections affect the prostate, specific bacteria are usually to blame. Understanding how these infections spread can help you make better choices about prevention and treatment.
The two most common bacteria linked to prostate infections are Chlamydia trachomatis and Neisseria gonorrhoeae. Both can move from the urethra into the prostate gland after sexual contact.
The process typically starts with unprotected sex. The bacteria first infect the urethra, then may travel upward into the prostate—even if urethral symptoms are mild or completely absent.
Chlamydia often causes few or no early symptoms, which means many men don’t realize they’re infected until complications appear. Gonorrhea, on the other hand, tends to produce more noticeable urethral symptoms, but it too can reach the prostate if left untreated.
The good news is that both infections usually respond well to antibiotics when diagnosed early. However, delays in treatment can raise the risk of prostate involvement and longer-term issues.
How Can You Protect Your Partner if You Have CP/CPPS?
Your transmission risk depends entirely on what's causing your prostate symptoms. This distinction makes all the difference for your partner's safety.
If You Have Bacterial Prostatitis
If your prostate infection is caused by an STI, there’s a real risk of passing the infection to your partner. The same bacteria that triggered your symptoms can still spread during sex.
That’s why it’s important to pause all sexual activity—including vaginal, oral, and anal sex—until both partners are properly treated. Even with condoms, there’s still some risk, since bacteria can be present in pre-ejaculate.
Both you and your partner should get tested and treated, even if no symptoms are present. Many STIs don’t cause noticeable symptoms, especially in women, so it’s possible to carry the infection without realizing it.
Before resuming sex, wait for medical clearance. Most healthcare providers recommend follow-up testing to make sure the infection is fully gone.
If You Have Chronic Pelvic Pain Syndrome
The good news for most men with prostate issues is that CPPS is not an infection and carries no risk of transmission.
You can’t pass CPPS to your partner through any kind of sexual contact. The condition causes inflammation and pain, but there are no infectious bacteria involved. From a safety standpoint, sex is not a concern.
That said, some men notice that sexual activity can trigger or worsen their symptoms. This is about personal comfort, not any danger to your partner.
Symptoms, Diagnosis, and Treatment of Prostate Infection
Recognizing prostate infection symptoms helps you seek appropriate care quickly. Early treatment often prevents complications and reduces discomfort.
Common Symptoms to Watch For
Prostate infection symptoms can vary significantly based on the type and severity. Key warning signs include:
- Pelvic pain, especially in the perineum (area between scrotum and anus)
- Testicular pain or discomfort
- Frequent urination, especially at night
- Urgent need to urinate
- Burning or pain during urination
- Fever and chills (particularly with acute infections)
- Lower back pain
- Pain during ejaculation
If you experience any of these symptoms, it's important to seek medical evaluation promptly to determine the cause and begin appropriate treatment.
How a Doctor Diagnoses the Cause
Proper diagnosis involves several key steps to determine the exact cause of your symptoms. It typically begins with a physical examination, including a digital rectal exam to assess the prostate for swelling or tenderness.
Next, urine tests are used to detect bacteria and white blood cells—common indicators of infection. In some cases, your doctor may collect urine samples both before and after a prostate massage to help localize the infection source.
If bacteria are found, culture tests are performed to grow and identify the specific organism. Although this process takes a few days, it helps determine the most effective antibiotic for treatment.
In more severe cases, such as acute bacterial prostatitis, blood tests may also be ordered to check for signs of a systemic infection.
Treatment Options
Treatment depends on what’s causing your symptoms, and the approach can vary.
If bacteria are present, you’ll need antibiotics. The specific type depends on your test results, and treatment usually lasts several weeks. In severe cases, you may need to stay in the hospital for IV antibiotics.
If you have CPPS, treatment focuses on relieving symptoms since there’s no infection. Doctors may recommend anti-inflammatory drugs, muscle relaxants, alpha-blockers, or pelvic floor therapy.
Other helpful options include heat therapy, prostate massage, and managing stress. Some men also feel better by avoiding spicy food, caffeine, and alcohol.
Frequently Asked Questions
Is a prostate infection always an STI?
No, most prostate infections are not sexually transmitted. Many bacterial infections come from urinary tract bacteria that spread to the prostate. The most common type, CPPS, isn't infectious at all.
Can a prostate infection be spread through oral sex?
While transmission through oral sex is theoretically possible with bacterial infections, it's less common than genital-to-genital contact. The main risk comes from direct contact with infected genital secretions.
Can chronic prostatitis be transmitted sexually?
This depends on the type. Chronic bacterial prostatitis caused by STI bacteria can potentially transmit to partners. However, CPPS—the most common chronic type—is not an infection and cannot be transmitted through sexual contact.
Navigate Your Prostate Health Journey with Prostate Health Store
Managing prostate health requires the right tools and support. Whether you're dealing with infection symptoms or focusing on prevention, quality products can make a significant difference in your comfort and recovery.
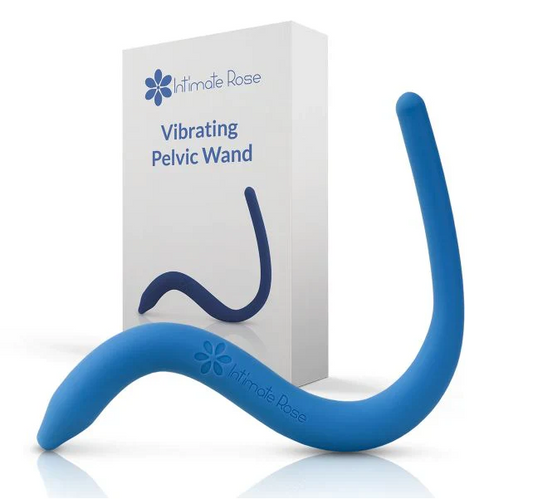
The Sonic Prostate Massager from Prostate Health Store provides therapeutic massage that may help reduce inflammation and improve circulation. This top-rated device offers a non-invasive approach to prostate wellness.
For comprehensive nutritional support, consider the Ultra Prostate Health Formula. This supplement combines saw palmetto, pygeum, and stinging nettle root with eleven essential nutrients to support overall prostate function.
Comfort during recovery is crucial, especially when dealing with pelvic pain. The Prostate and Pelvic Floor Support Cushion provides targeted relief by reducing pressure on sensitive areas while sitting.
Order now and take charge of your prostate health with trusted, professional-grade tools made for men’s comfort and recovery.